While physical activity may lower the risk of developing dementia, it also plays a crucial role in reducing mortality for those already diagnosed with the condition. Engaging in regular exercise can improve cardiovascular health, mobility, and overall resilience, which may help prolong life and enhance quality of life for individuals with dementia.
Dementia significantly reduces life expectancy, with a median survival time of around 4 to 5 years after diagnosis (link). As current medications cannot reverse dementia, non-pharmacological strategies, particularly lifestyle modifications like physical activity (PA), have become essential for managing disease progression and reducing mortality risk. Past research suggested that regular physical activity, such as exercising over 150 minutes per week, is linked to a decreased mortality risk in dementia patients, with a 36% reduction observed among cognitively frail elderly populations. Additionally, higher cardiorespiratory fitness levels correlated with lower dementia-related mortality. However, these previous studies largely focused on single-time PA measurements, leaving a gap in understanding the effects of changes in PA levels before and after a dementia diagnosis on mortality risk.
A new study used data from South Korea’s National Health Insurance Service (NHIS) to analyze the impact of physical activity (PA) on mortality in individuals newly diagnosed with dementia between 2010 and 2016. Researchers included 60,252 dementia patients who self-reported their PA levels during routine health check-ups. The average participant age was 74, with most having Alzheimer’s disease (72%) or vascular dementia (12.5%). PA was categorized by intensity (light, moderate, vigorous) and frequency, based on a questionnaire. The activity classification was based on metabolic equivalents (METs). One MET is defined as the amount of energy expended while sitting at rest (which loosely corresponds to your basal metabolic rate); light activities are < 3 METs; moderate activities are 3-6 METs, and vigorous activities are > 6 METs. An example of light physical activity is walking for over 30 minutes. Participants were grouped by changes in activity levels during the course of the study: Non-exercisers (78%), Quitters (10%), Starters (8%), and Maintainers (3.5%); in other words, only 3.5% of subjects maintained exercise levels over the study period. Results were analyzed for overall and intensity-specific PA, with findings interpreted in terms of risk reduction in all-cause mortality, adjusting for covariates like age, sex, health conditions, and lifestyle factors.
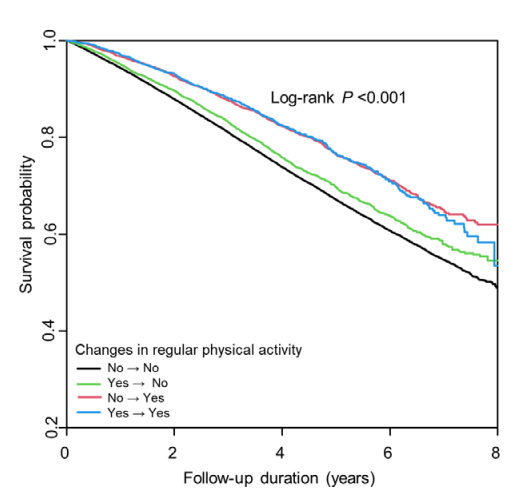
During an average follow-up period of 3.7 years, 27.3% (16,431) of participants died (which is roughly consistent with a median survival of 4 to 5 years). Among the 60,252 participants, those who maintained regular PA before and after their diagnosis (regardless of intensity) had the highest survival rates with a Hazard Ratio (HR) = 0.71 compared to inactive individuals. Patients who started PA after diagnosis also benefited, though slightly less than Maintainers; starting any PA intensity post-diagnosis was linked to ~25% reduction in mortality risk (Figure 1).
There was a dose-dependent relationship with mortality risk decreasing progressively with higher PA. Those engaging in ≥1000 MET-min/week showed the largest reduction (HR=0.66) in all-cause mortality (p<0.001 for the trend).
One of the primary lessons of the study was that maintaining any level of PA, including light activities, can be beneficial, especially for dementia patients who may face challenges in sustaining higher-intensity exercises. In addition, starting PA after diagnosis leads to a significant reduction in mortality. It is important to acknowledge the limitations of the study which include reliance on self-reported PA, potential recall bias, and unaccounted for confounders associated with increased physical activity. Nevertheless by assessing PA at multiple time points in the study, researchers could show the benefits of consistent PA as well as demonstrating a dose-response relationship.
In summary, public health efforts should prioritize reducing sedentary behavior and promoting regular PA among individuals with dementia, as even low levels of activity can contribute significantly to health and longevity.
Figure 1. Kaplan-Meier survival curves after dementia diagnosis (all-cause dementia). The four curves represent changes in physical activity before and after diagnosis. No => No, Non-exercisers; Yes => No, Quitters; No => Yes, Starters; Yes => Yes, Maintainers. These curves are unadjusted for covariates (from Figure 2 of Park et al. BMJ Sports Medicine, 2024).
No comments:
Post a Comment